COVID-19 continues to show signs of retreat in the Bay Area, even though public health officials will continue to cautiously tell us "we aren't out of the woods" probably for a few months more. And UCSF's Dr. Monica Gandhi has penned a piece explaining what the next few months and years may look like as the virus lingers.
We learned the harsh lesson in July that all of June's positive trajectory and exuberant reopening could quickly be quashed by this pandemic's own unpredictability. So it's wise not to make any bold pronouncements or predictions until all the evidence is in.
But San Francisco's daily new case numbers continue to go down fairly steadily. Last week's seven-day average of daily new cases in the city was 76 (as of Sept. 26), down from a high of 309 in early August. And the number of new cases among vaccinated residents continues to slide, with the daily average now at 7.3 cases per 100,000 vaccinated residents — compared to 14.4 cases per 100,000 unvaccinated residents. The city is now 75% fully vaccinated across all ages, and the percentage goes up to 88% for all eligible ages (12 and up) with at least one dose.

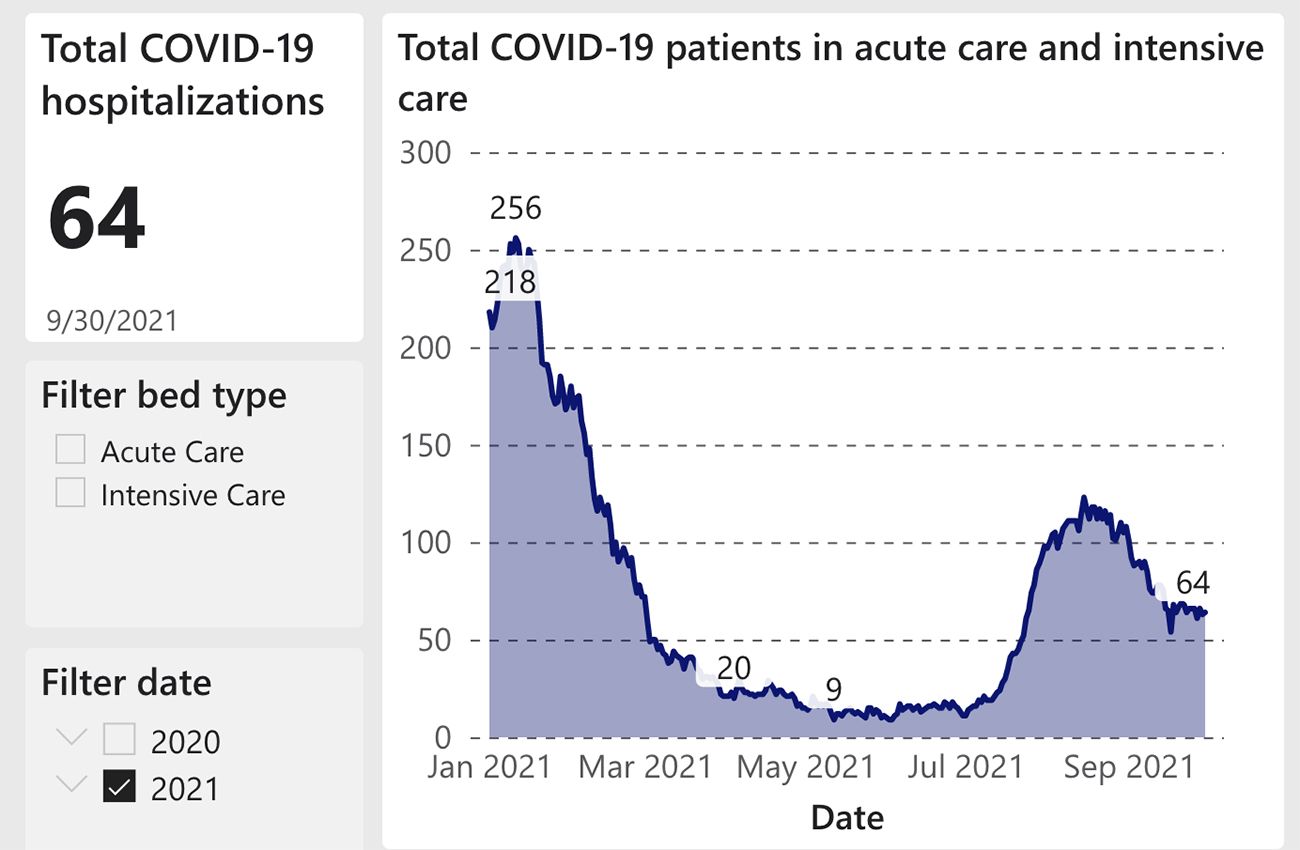
Hospitalizations, both in SF and across the Bay Area, are also steadily going down, though August and September saw a surge in both hospitalizations and deaths from the Delta surge. San Francisco had 64 COVID patients in hospitals as of Thursday, September 30, while the overall numbers of hospitalizations across the state and region continue to go down in parallel with declining new case numbers.
Measures like mandatory indoor masking and checking vaccine status at the door of all bars, clubs, and restaurants has likely helped in bringing case numbers down since the Delta surge began in July — and a segment of the population is now double-immune from both a vaccine and a recent Delta-variant breakthrough infection. This may mean that the local mask mandate will once again be loosened in the coming days or weeks, but that remains to be seen — and we'll likely be encouraged to keep the masks on us for public transportation and Ubers for the foreseeable future.
As you should know by now, "herd immunity" is not going to provide perfect safety from infection with this virus, but it will likely keep most people out of the hospital. And we're not talking about eradicating COVID-19, meaning that it will likely be endemic and create little outbreaks and surges across the globe for years.
"An epidemic of COVID-19 in the Bay Area becomes endemic when the disease is manageable locally (e.g., not causing an undue burden of hospitalizations or health care utilization) but is not likely to be eliminated due to inherent properties of the pathogen," writes Dr. Monica Gandhi, an infectious disease specialist at UCSF, in a new Chronicle opinion piece.
One factor that will drive the endemic nature of COVID, Gandhi says, is the fact that the disease can still be carried by animals. So, unlike smallpox, which animals can't carry, COVID is likely to stick around in pockets no matter how immune the world population becomes. And the infectious nature of this virus in patients who are asymptomatic or pre-symptomatic will make it continually hard to isolate.
It's a disease, therefore, that will have to be managed through mass-vaccination, and infections will become more treatable over time with the use of antivirals — like the oral medication Merck says has already shown promise in reducing severity of the disease.
"The key to this normalcy is immunity, preferably through vaccination and not natural infection," Gandhi says. And she notes that a vaccine-resistant variant is unlikely to emerge due to the documented breadth of the body's T-cell response to the vaccines.
Meanwhile, the CDC is (unrealistically) telling people once again to avoid holiday travel this year, particularly for the unvaccinated.
And while COVID case numbers are going down in most of the nation, the Delta surge has now hit Alaska, and the hospital-bed situation there has hit crisis levels. Also, as the New York Times reported over the weekend, Alaska is a hotbed of anti-vaxx craziness, with some anti-vaxxers having recently worn yellow Stars of David to public meetings to make a comparison between the vaccine campaign and the Holocaust. So that state's COVID troubles are likely far from over.
With ICU beds in short supply, the Times reports, doctors in Alaska have begun making the kind of grueling choices that others around the country had to make last year in the pandemic's height about which patients will receive life-saving care and which will be left to die.

